29 year old male patient . Daily labour by occupation , resident of Bhongir came with
Chief complaints
Pain abdomen 10 days
Vomitings 10 days
Involuntary movements of left upper limb 1 week
History of present illness
Patient was apparently asymptomatic 10 days ago then he developed pain abdomen 10 days ago which was sudden onset in epigastric region , sharp which is radiating towards back , aggrevating on taking foods.
• H/o 2 episodes of vomiting which is non bilious non blood tinged , non projectile water as content .
• H/o seizure , involuntary movemnt of the left upper limb a/w Deviation of mouth to right side uprolling of eyes , drooling of saliva
H/o Loss of conciousness for almost 15 mins and regained his conciousness.
H/o Slurring of speech
H/o Memory loss
No H/o Trauma ,
No H/o Neck stiffness ,
No H/o Fever ,
No H/o weakness
No H/o Loose stools involuntary micturation or defecation
History of past illness
Patient had pain abdomen and 2 episodes of vomiting for which he was admitted in local hospital he had an 1 episode of involuntary movemnents ,
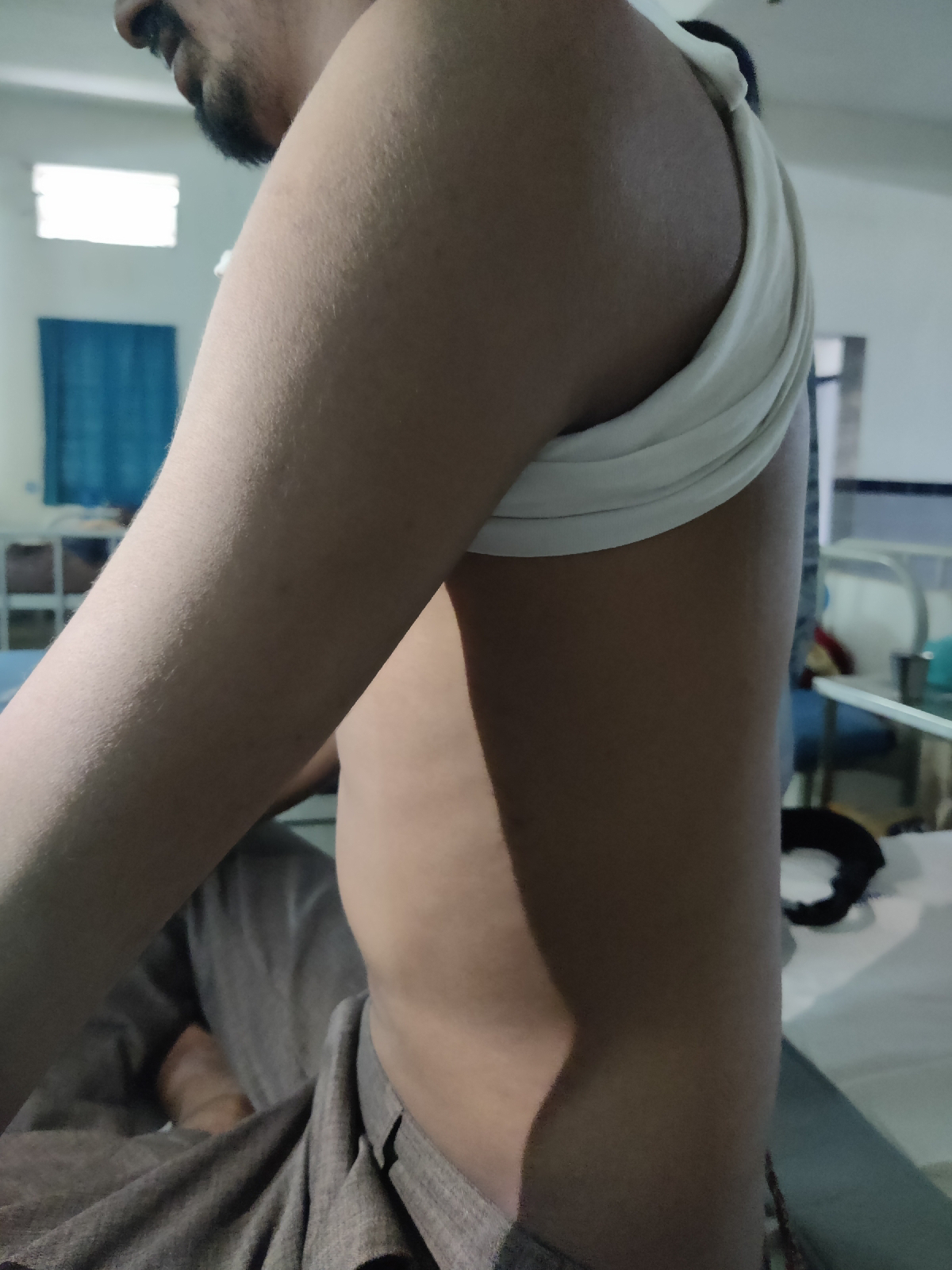
- history of Left shoulder disslocation during his seizures.
- N/k/c/o HTN, DM ,TB,BA,CVA,CAD, Thyroid disorders .
Surgical History
Pt underwent Surgery for Hernia
Drug allergies
Not significant
Family History
No H/o seizures in family
Personal History
Diet - Mixed
Appetite - Decreased
Sleep - Decreased
Bladder & Bowels - Irregular
Addictions - Alcoholic since 10 years Whiskey 500 ml daily . and experience palpitations tremors in its absence for 3 days
General examination
Patient is concious , coherent , cooperative to time place person
Pt is Moderately built & moderately nourished
No Pallor -
No icterus
No cyanosis
No lymphadenopathy
No koilonychia
No pedal oedema
Vitals
Temperature afebrile
Bp - 130/90 mmhg
RR - 20 cpma
HR - 93 bpm
Spo2 - 99% on RA
Height 160 cms
Weight 60kgs
Systemic examination
CENTRAL NERVOUS SYSTEM
Pt is C/C/C
HMF - Intact
Speech & language – Normal
Memory can recall
No Signs of Meningeal irritation
Motor and sensory system – Normal
Reflexes – Normal
Cranial Nerves – Intact
Gait – Normal
Cerebellum – Normal
GCS Score – 15/15
CRANIAL NERVE
OLFACTORY - NORMAL (SMELL)
OPTIC - Normal
OCCULOMOTOR - Normal
TROCHLEAR Normal
TRIGEMINAL Normal
ABDUCENS Normal
FACIAL NERVE Normal
VESTIBULOCOCHLEAR Normal
GLOSSOPHARYNGEAL Normal
VAGUS - Gag reflex present
SPINAL ACCESSORY Normal shrugging shoulders
HYPOGLOSSAL Normal ( Not deviated )
MOTOR SYSTEM
Bulk -
Right. Left
Tone UL 5/5 Unable to perform due
to his pain
LL. 5/5 5/5
Power. UL 5/5. Unable to perform due
to his pain
LL 5/5 5/5
REFLEXES
Corneal - N
Conjuctival - N
Pharyngeal - N
Palatal -N
Abdominal -N
Cremasteric - N
DEEP TENDON REFLEX
Jaw Jerk - N
Biceps - N
Triceps - N
Supinator - N
Knee jerk - N
Ankle jerk- N
Clonus - absent
Position sense:
Right Left
Upper Limb 10/10 unable to perform due to his pain
Lower Limb 10/10 10/10
-Graphaesthesia-Postive
-Stereognosis-Positive
Cerebellar signs:
-Titubation:absent
-Nystagmus:absent
-Dysarthria:absent
-Hypotonia:absent
-Intention tremor:absent
-Coordination
a.Finger Nose test: Normal
b.Heel Knee test: Normal
c. Dysdiadokokinesia: Negative( able to perform rapid alternative movements)
Signs of Meningeal Irritation:
Neck stiffness: absent
Kernig’s sign :absent
Brudzinski’s sign:absent
CARDIOVASCULAR SYSTEM
INSPECTION
Chest is elliptical shaped, bilaterally symmetrical.
Trachea appears to be central
Movements are equal bilaterally
JVP:Raised
No Visible epigastric pulsations
No scars or sinuses
PALPATION
All the inspectory findings are confirmed
Trachea is central
Apical impulse felt at 5th intercostal space lateral to midclavicular line.
AUSCULTATION
S1 S2 heard no murmurs
RESPIRATORY SYSTEM
INSPECTION
Chest is elliptical shaped,
bilateral symmetrical.
Trachea is central
Movements are equal bilaterally
No Visible epigastric pulsations
No scars or sinuses
Apical impulse not seen
PALPATION
All inspectory findings are confirmed: Trachea is central, movements equal bilaterally.
Antero-posterior diameter of chest >Transverse diameter of chest
Apex beat felt in 6th intercostal space lateral to midclavicular line
PERCUSSION
Resonant note heard in all areas bilaterally
AUSCULTATION
Bilateral air entry present – Normal vesicular breath sounds heard
PER ABDOMEN
INSPECTION
Shape of abdomen appears to be scaphoid
No Visible epigastric palpations
No engorged veins sinus scars
PALPATION
All inspectory findings conformed
Tenderness +
Palpable mass near left Hypochondrium
No organomegaly
PERCUSSION
Tympanic note heard all quadrants abdomen
AUSCULTATION
Bowel sounds heard in RIF
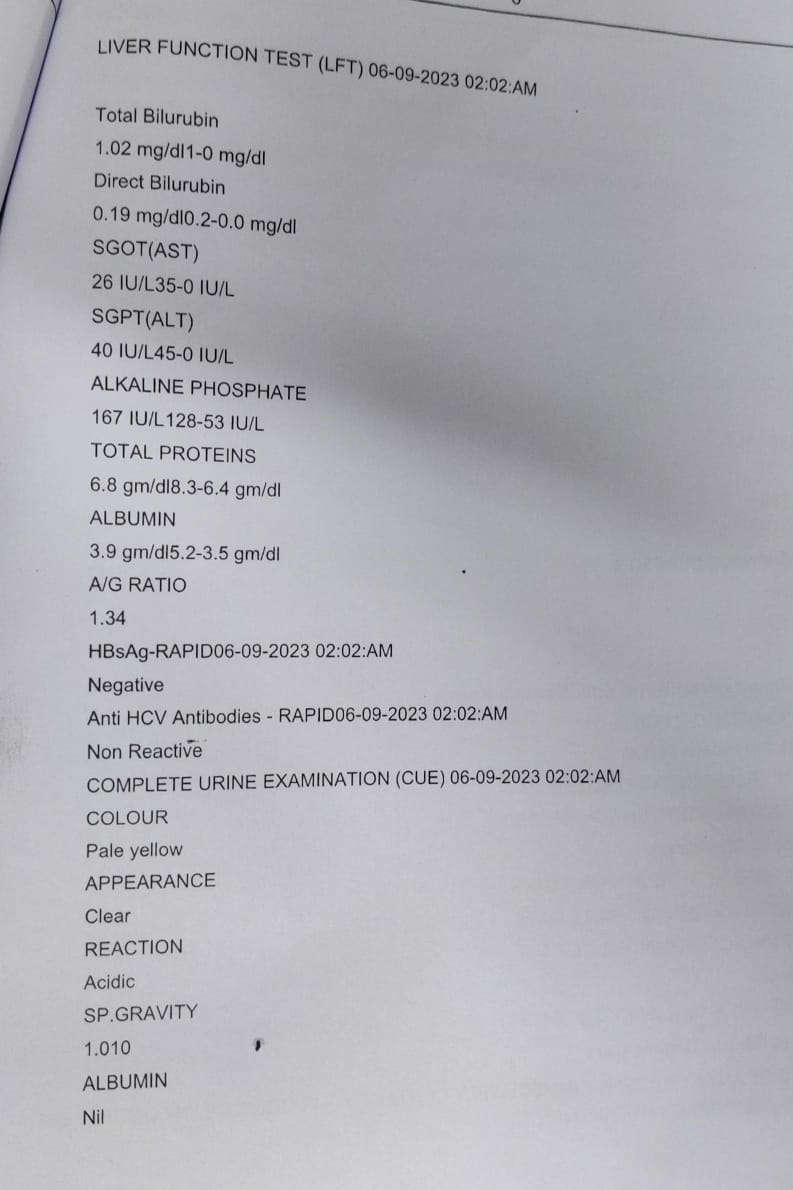
CLINICAL IMAGES
Provisional Diagnosis
? Acute pancreatitis
? Alcoholic gastritis
DIAGNOSIS
Focal seizures










Comments